Migraine is an inherited tendency to have headaches with sensory disturbance. It’s an instability in the way the brain deals with incoming sensory information, and that instability can become influenced by physiological changes like sleep, exercise and hunger.
Migraines can vary in severity and symptoms depending on the type experienced. The different types of migraine include:
- Migraine with aura
- Migraine without aura (most common)
- Chronic migraine
- Vestibular migraine (affects balance and symptoms may include vertigo)
- Abdominal (includes severe stomach pain for 2-72 hours and sickness, though no headache during the attack).
- Menstrual migraine
Why are you getting migraines?
While the actual mechanisms behind migraines are not yet fully understood, common triggers and risk factors have been identified. If you suffer from migraines, it can be helpful to identify what triggers them so that you can reduce or better manage them. One way to do this is to keep a diary of your diet, activity, stress levels and symptoms. I know it sounds a lot but over time you will hopefully be able to identify patterns and be able to take action specific to them to see if they help.
Below are explanations of some of the common triggers:
Stress
Perhaps one of the best known migraine triggers. Stress can disrupt brain functions and increase cortisol (the stress hormone) levels. Beyond this, stress can also influence our behaviours resulting in less healthful diet and lifestyle choices, which may trigger or exacerbate the migraine symptoms.
Diet
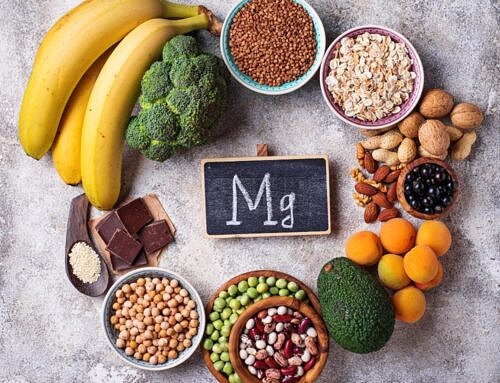
While skipping meals can result in low blood sugar and may therefore trigger migraines, not having enough of certain vitamins, minerals and proteins in the diet may also contribute. Such nutrients include magnesium, taurine and tryptophan (see later).
In addition, drinking too much caffeine may trigger migraines – but so too may caffeine withdrawal! If you want to reduce your caffeine intake, it may be helpful to do so gradually.
Alcohol may also be a trigger, although you may find that it is the quantity and/or specific alcoholic drinks rather than alcohol itself.
Dehydration. Not getting enough fluids, or having too many diuretics such as caffeine and alcohol, can trigger migraine symptoms. Take particular care in hot weather or if taking medications (always read the information leaflets and speak to your doctor/pharmacist if you have concerns). You can easily monitor your level of hydration by checking the colour of your urine – you want it a pale straw colour rather than a dark.
Lifestyle
Lifestyle choices such as regular strenuous exercise may result in migraines due to overexertion.
Also, having insufficient quantity or quality of sleep may result in migraines. This can also be the case if your sleep routine is irregular due to its impact on your circadian rhythm.
Oestrogen
Lowered oestrogen levels can trigger migraines, possibly due to its influence on serotonin and/or the part of the nervous system involved in pain signalling. Unfortunately, this is a regular occurence as part of the menstrual cycle, so some females experience migraines on a monthly basis. It may also happen as a result of the menopause or hormonal contraception.
Light sensitivity
Sensitivity to bright or fluorescent lights may trigger migraines.
Individuals who suffer allergies such as hayfever that irritate the eyes may find they are more vulnerable during the time of allergic reactions.
Some health conditions
Some health conditions may contribute to recurring migraines. These include Coeliac disease, H-pylori infection, insomnia, fibromyalgia, Behçet’s disease and epilepsy.
Gut health
You may be familiar with the phrase “gut-brain axis” in relation to stress, but did you know it may also have a role in migraines? A review study in 2020 by Arzani, et al, explained that someone who has suffered migraines for a long time may have a higher chance of being diagnosed with IBS. While the specifics of how they are connected is not yet confirmed, probable influences include inflammation, the microbiome balance, nutrition, and hormonal links. It is also believed that activities in the brain affect the gut.
Thinking about the gut microbiome more specifically, it is thought that short-chain fatty acids (SCFAs) produced by gut bacteria may reach the brain and have protective properties. SCFAs are produced by the bacteria digesting fibre in the colon.
Our chemical messengers
Neurotransmitters are the chemical messengers that carry signals between nerve cells, muscles and glands. They are important throughout the whole body, including the brain.
One such neurotransmitter is glutamate, stimulates the nerve cells in the brain and also converts into another neurotransmitter (GABA) needed for sleep and muscle function. While this all sounds really positive, it needs to be kept in balance –
- a high level may contribute to migraines and/or digestion-related conditions.
- a low level may result in brain fog, low energy, and a lack of focus.
Although we make glutamate in the body, we also get it from our food. Therefore if you experience these symptoms regularly it may be worth considering which of these foods you eat and how often:
- monosodium glutamate (MSG) often found as an ingredient in processed foods such as stock cubes, sauces, dressings and soups
- meat and seafood, including tuna and scallops
- milk and cheese
- tomatoes, mushrooms, peas, potatoes
- fermented beans
- yeast extract
- hydrolysed vegetable proteins
Protein processes
One of the proteins that we make within the body is cholecystokinin (CCK). It is involved in several stages of digestion, as well as behaviour and mood. While the mechanisms are not yet fully understood, scientists believe that increased levels of CCK contribute to migraines. This happens by increasing the brain’s sensitivity to pain and light, and may increase symptoms associated with stress and anxiety.
Another protein that is thought to contribute to migraines is tryptophan. We process this protein in the body to produce two substances that affect the brain: serotonin (also processed into melatonin) and kynurenic acid. However, only very small amounts of kynurenic acid are able to reach the brain. In contrast to CCK, it is reduced levels of tryptophan that have been found to induce the headache experienced during migraines as well as nausea and dizziness. The symptoms are not thought to be due to the level of the protein itself, but due to the lower serotonin levels that reduce from its depletion.
Risk profiles
You are at increased risk of migraines if you are female, aged between 25 and 55 years, white and/or have a lower socioeconomic status. You are also more likely to experience migraines if you have a family history of them.
Migraines have been found to be more frequent and severe in individuals who are significantly overweight (obese).
What can you do if you suffer from migraines?
With so many potential causes and triggers of migraines, it may seem like there is little you can do to help your symptoms beyond medications. But, there are evidence-based nutrition and lifestyle strategies that may help you to support your health and wellbeing.
Finding out your triggers is a great starting point in managing migraines. Unfortunately, they won’t always be obvious or easy to avoid. To help you identify or manage triggers you could try:
- Boosting your intake of nutrients that support neurological health such as taurine, tryptophan and vitamin B6. Good sources include red meat (not cured or industrially processed), turkey, seafood, oily fish (e.g. salmon), tuna, eggs, nuts and seeds, cheese, tofu, fruit and veg, and fortified foods.
- Including more magnesium-rich foods such as dark chocolate (70%+), wholegrains, leafy greens, nuts, seeds, beans, fatty fish and avocados.
- Avoiding large, high-fat meals.
- Avoiding common trigger foods such as aged cheeses and processed meats.
- Ensure you have a fibre-rich diet to support your gut health.
- Ensure you get sufficient, good-quality sleep
- Reduce your exposure to bright or flurorescent lighting if you are light sensitive.
Coenzyme Q10 (CoQ10) is another nutrient thought to have a role in migraines. We make this in our body using the same enzyme that we use to make cholesterol. Taking statins may therefore interfere with its production – speak to your doctor or pharmacist if you are taking statins and have concerns. However, there are also dietary sources such as organ meat, meat (pork, beef, chicken), fatty fish, legumes, nuts and seeds.
To help work out your triggers, it is a good idea to try one change at a time for several weeks. If you find the undesirable effect of increased migraines when increasing any of the suggested foods, stop them. They may be your triggers!
To help manage your stress levels you might try:
- Practising meditation, yoga or pilates regularly.
- Spending time outdoors, particularly in woodland, the countryside or near water.
- Taking time to breathe – even just concentrating on your breath for a moment can give you a moment to calm your mind and think more clearly.
- Improving the quantity and quality of your sleep.
- Reducing your caffeine and sugar intake (I know those are emotional and energy go-tos, but they can have a negative effect in the longer-term).
- Temporarily removing yourself from causes of acute stress may allow you to calm yourself and clear your mind, allowing you to think more clearly when you return to the issue.
References/Further Reading
Magnesium in Neuroses and Neuroticism – Papadopol and Nechifor (2011) – https://www.ncbi.nlm.nih.gov/books/NBK507254/#:~:text=Magnesium%20can%20directly%20reduce%20dopamine,of%20glutamate%20on%20dopamine%20release.
Migraine and Obesity@ Epidemiology, Possible Mechanisms, and the Potential Role of Weight Loss Treatment – Bond, et al (2012) – https://pmc.ncbi.nlm.nih.gov/articles/PMC2974024/#:~:text=In%20this%20study%2C%2018%2C968%20of,%2Dweight%20group%20(6.5%25).
Exploring the Tryptophan Metabolic Pathways in Migraine-Related Mechanisms – Körtési, Spekker and Vécsei (2022) – https://pmc.ncbi.nlm.nih.gov/articles/PMC9736455/#:~:text=Tryptophan%20and%20Its%20Role%20in%20Migraine&text=Some%20research%20groups%20observed%20decreased,and%20migraine%20(Figure%201).