1) Digestion
Starting with the most obvious, the gut is key to our digestion. Starting in our mouths, down to our stomachs, through the small intestine and into the colon, the upper and lower parts of our gut help us to digest our food. But did you know that each part has a role to play in the absorption of nutrients as well as breaking down the food?
In the mouth, saliva begins the process of breaking down carbohydrates. The longer you chew the sweeter food may taste and the better broken down it will be – it is generally said we should chew our food 20 times before swallowing.
In the stomach our food gets mixed with other digestive juices which breakdown the food further, and help us to absorb nutrients such as protein and vitamin B12. This is part of the reason why it is important to have the cause of recurring reflux or heartburn investigated, not just rely on antacids or other medications to help you feel better (they have their place of course, but it is better to address the cause if possible).
We then get on to the small and large intestines, and it isn’t all about poo. This doesn’t really become a thing until the very end of the digestive process. Through the intestines further processing happens with nutrients being absorbed through. The image below illustrates the intestines and where the different nutrients are absorbed as the food continues through the tract.
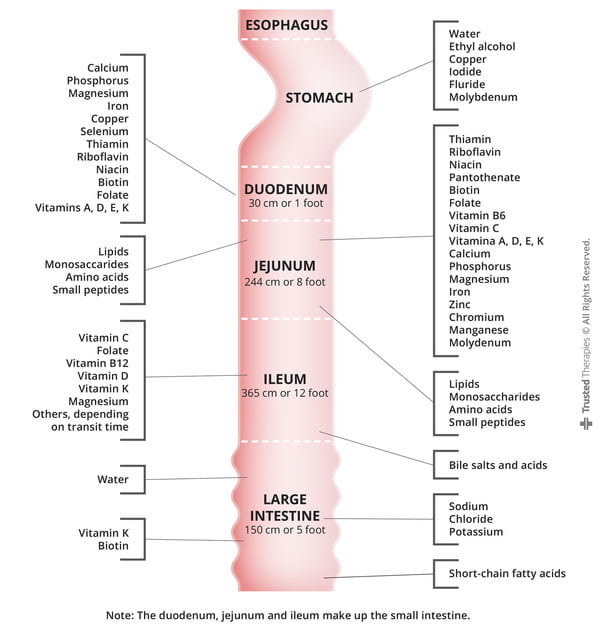
Source: Absorption of nutrients across intestines – About A Dietitian. https://aboutadietitian.wordpress.com/gastroenterology-and-nutrition/absorption-of-nutrients-across-intestines/
2) Immunity
It is now believed that 70-80% of our immune system is in the gut. That’s right, not in our blood (although that is still an important part), but in our gut. There are parts of the immune system in our mouths (saliva), stomach (stomach acid), liver (Kupffer cells) and the intestines.
To expand on the role of the intestines, the microbiome (see below) helps our cells to recognise health threats and trigger the appropriate immune reaction. This is happening all the time, and the better the immune system works the less risk there is that we will notice it through illness.
Furthermore, the large and small intestines are lined with a thin barrier that is intended to stop microbes (or other unwanted things) getting through to the rest of our body. The theory of intestinal permeability explains that substances that are normally trapped by the barrier (such as food proteins) are able to pass through and may trigger allergic reactions. Increased permeability is seen in individuals with irritable bowel disease, and may also be associated with type 1 diabetes, asthma and autism. The level of gut permeability may be affected by stress or infection. Research into these associations and causes continues.
The gut is believed to have a huge role in autoimmunity too, with the potential that it may be associated with gut microbes breaching the intestinal barrier.
3) The Microbiome
Did you know that scientists now believe we have more bacteria inside our bodies than on the outside? ‘Eeeew’ is probably your first thought here – but stay with me! It isn’t a bad thing. Despite our behavioural conditioning over several decades, not all bacteria is bad. In fact a lot of it is good and useful, in the right place. The biggest problems with internal bacteria are when they spread to the wrong place (for example with small intestine (SIBO)) or they are out of balance. There are whole books written about this topic, so I am only going to give you a snippet of the information available about this important system.
The population of our large intestine’s microbiome begins at birth. We received bacteria from our mothers during natural birth. With caesarian sections this is reduced as the process is clinically sterile (necessary to avoid infection), however there are now some hospitals introducing vaginal swabs which, without too much detail, expose the baby to the mother’s microbiome and begins the process of establishing the microbiome. From then on, the microbiome is affected by whether we are breastfed or formula fed, the first foods we eat, and the places we visit and play. It continues throughout our lives being affected by our ongoing diet, our environmental exposures, and our medications (especially antibiotics – again they have their place, but this is a good reason for their use to be controlled and not taken for things they aren’t designed for like cold viruses). Differences in the health of the microbiome have been identified between people of a healthy weight and those who are classified as obese – which circumstance contributes to which however, has not been established.
So, why does it matter? The balance of bacteria in our guts is important to our digestive system (it helps use to breakdown and absorb some nutrients, AND make some nutrients), metabolism of medications, maintenance of the intestinal barrier, and our immune system.
4) Link to the Brain
Butterflies in your stomach? Need the toilet more when you are nervous? Headaches? These can all be signs of how the gut and the brain are connected. The gut-brain axis.
Essentially, the gut is connected to the brain via the nervous system, with the vagus nerve being one of the biggest nerves sending messages to and from each area. They are also connected via chemicals produced in the gut. For example, the neurotransmitter serotonin.
Short Chain Fatty Acids (SCFAs) are also produced in the gut during the digestion of fibre. These are important for brain function, including appetite control and maintenance of the blood-brain barrier.
The gut’s role in the immune system is also believed to also help protect the brain by limiting inflammation, and protecting the body from harmful microbes.
5) Food and Drink
Looking after our gut is clearly important, and there are things we can do to look after it. I’m not going to detail the environmental exposures etc here, but cleaning everything with commercial anti-bacterial cleaners all of the time may not be the best thing to do (like everything, anti-bacterials have their time and place!). White vinegar and lemon juice are great traditional cleaning products.
What I do want to have a quick look at is food and drink. Ensuring we have enough fluid helps to keep things moving, so to speak. A general guide is to aim for 1.5-2 litres of (non-alcoholic) fluid a day. Ideally the fluid level includes water but it can also come from foods such as fruit, vegetables and soups.
To keep the bacteria happy and to develop and maintain a healthy balance we need to eat a healthful, varied diet:
- avoid foods containing added sugar
- ensure you include a good amount of fibre each day (health guidelines suggest we need 30g per day), including whole grains such as oats
- eat leafy greens each day
- eat a range of fruit and vegetables each day (aim for the rainbow)
- reduce or eliminate ultra-processed food
- include fermented foods (yoghurt, kefir, sauerkraut)
- include sources of omega-3 such as oily fish. flaxseed (linseed) and walnuts.
Don’t forget – everything detailed above affects us all, young and old. It is therefore important that we look after not only our guts throughout our lives. Teach children healthful habits when they are young and their guts will thank you into adulthood.
References/Further Reading
- Absorption of nutrients across intestines – About A Dietitian. https://aboutadietitian.wordpress.com/gastroenterology-and-nutrition/absorption-of-nutrients-across-intestines/
- The role of gut microbiota in immune homeostasis and autoimmunity – Wu and Wu. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3337124/#:~:text=The%20gut%20microbiota%20that%20resides,dysregulation%2C%20leading%20to%20autoimmune%20disorders
- Possible links between intestinal permeability and food processing: a potential therapeutic niche for glutamine – Rapin and Wiernsperger. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2898551/



